 Getty Images
Getty ImagesMutations in these regions of so-called ‘junk’ DNA are increasingly linked to a range of diseases, from Crohn’s disease to cancer.
Since the Human Genome Project was declared complete in 2003, scientists have been trying to pinpoint new areas among the three billion letters of our genetic code that may play a crucial role in disease.
Using technologies that allow whole genome samples to be analyzed faster and cheaper than ever before, vast numbers of genome-wide association studies – called GWAS – have been published, identifying genetic variants linked to various chronic diseases.
Frustratingly for many geneticists, this turned out to be the easy part. The much harder part is understanding how they are relevant. For example, while GWAS has identified DNA segments linked to inflammatory bowel disease 215 different chromosomal locationsscientists have only managed to pinpoint the exact mechanisms involved in four of these mechanisms.
One of the biggest challenges is that many of these pieces of DNA are located in so-called gene deserts, parts of the genome that initially seemed to contain nothing relevant – genetic ‘junk’ that could be ignored. After all, less than 2% of the human genome is dedicated to coding genes that produce proteins, while much of the remaining 98% has no clear meaning or purpose.
“You’ll say, ‘Oh, here’s a really important association and it increases your risk for a lot of different diseases,’” says James Lee, a physician-scientist who leads a research group at the Francis Crick Institute in London. “But when you actually look at that piece of DNA, there’s just nothing there.”
 Getty Images
Getty ImagesFor years, gene deserts have been one of the most confusing areas of medical science, but scientists are slowly gaining information about their apparent purpose and why they exist.
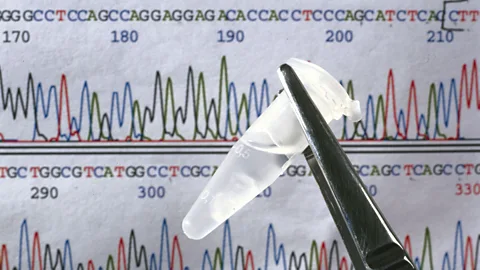
Recently, Lee and colleagues at the Crick Institute published a new research in a specific gene desert known as chr21q22. Geneticists have known about this gene desert for more than a decade, as it has been linked to at least five different inflammatory diseases, including inflammatory bowel disease.IBD) to a form of spinal arthritis known as ankylosing spondylitis. Yet deciphering its function has always proven elusive.
For the first time, however, the Crick scientists were able to show that chr21q22 contains an enhancer, a DNA segment that can regulate nearby or distant genes, increasing the amount of proteins they make. Lee calls this behavior “a volume knob.” When they dug deeper, they discovered that this enhancer is only active in white blood cells called macrophages, where it can increase the activity of a previously little-known gene called ETS2.
Although macrophages play a crucial role in clearing away dead cells or fighting harmful microorganisms, when the body produces too many they can wreak havoc in inflammatory or autoimmune diseases, invading affected tissues and secrete harmful chemicals that attack them. The new study showed that when ETS2 is boosted in macrophages, it enhances virtually all of their inflammatory functions.
Lee describes it as “the central orchestrator of inflammation.” “We’ve known for a while that there must be something at the top of the pyramid that tells the macrophages to behave this way,” he says. “But we never knew what it was. The most exciting thing about this is that if we can somehow target it, we might have a new way to treat these diseases.”
 Getty Images
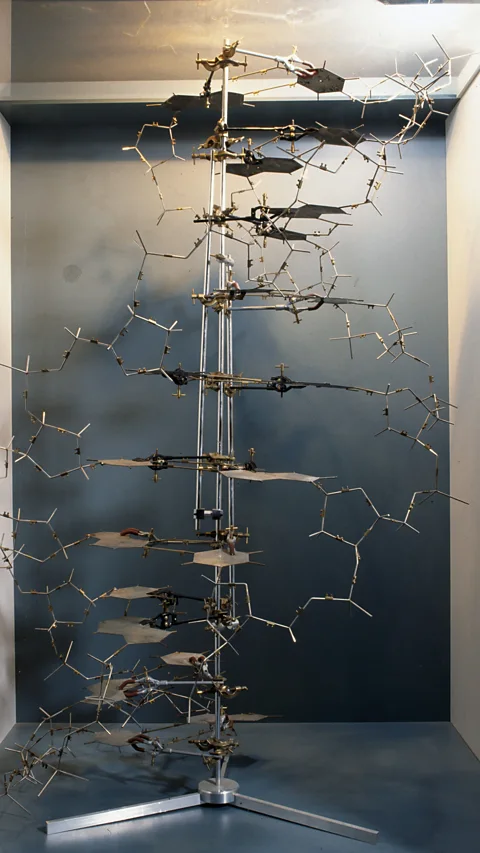
Getty ImagesBut if gene deserts can cause us so much harm, why are they in our DNA?
Going back in time, Lee’s colleagues at Crick’s Ancient Genomics Laboratory were able to show that the disease-causing mutation in chr21q22 first entered the human genome sometime between 500,000 and a million years ago. This specific DNA change is so old that it was even present in the genomes of Neanderthals and in some ancestors of Homo sapiens.
It turns out that its original purpose was to help the body fight foreign pathogens. Before antibiotics were invented, being able to quickly initiate an increased inflammatory response via ETS2 was extremely useful. “Within the first few hours of seeing bacteria, your macrophage responses are amplified,” says Lee.
As a result, completely blocking ETS2 could leave IBD patients vulnerable to future infections. However, Lee says that when activity is reduced by 25 to 50%, it appears to be able to produce a profound anti-inflammatory effect without risking putting the patient under too much immunosuppression. Although this theory has yet to be tested in clinical trials, the researchers showed that MEK inhibitors – a class of cancer drugs that can dampen ETS2 signaling – were able to reduce inflammation not only in macrophages, but also in intestinal samples taken from people with IBD.
This appears to represent a new route to an entirely new class of treatments for IBD patients. “Some of these MEK inhibitors have side effects, and what we’re trying to do now is make them more targeted and safer, so that for lifelong diseases like IBD, we can actually offer patients a drug that turns off the inflammatory process and actually makes them a lot better.” , says Lee.
Now Crick’s researchers are turning their attention to the other four diseases that have been linked to the chr21q22 gene desert, to see if altering ETS2 activity can also help alleviate the excess inflammation that seems to cause the condition.
“One of the most important is an inflammatory liver disease called primary sclerosing cholangitis,” says Lee. “It is a particularly nasty disease because it can cause liver failure, causing people to need transplants. It can also have a much higher risk of causing liver cancer, and this can happen in young people. And at the moment there is no single cure that It has been shown to work, but there is little to offer patients,” he says.
From cancer to lupus
Scientists also predict that studying gene deserts will provide vital information that will help improve our understanding of the different pathways involved in tumor development.
Cancer researchers, for example have confirmed a gene desert called 8q24.21 is known to contribute to cervical cancer because the human papillomavirus, the main cause of the disease, harbors in this part of the genome. In doing so, the virus amplifies a gene called Myc, a known cause of cancer. Studies suggest that the link between 8q24.21 and Myc may also play a role in a number of ovarian, breast, prostate and colorectal cancers.
Richard Houlston, from the Institute of Cancer Research in London, says several genetic variants have been found in gene deserts and have been found to contribute to the hereditary risk of common cancers. Knowledge of these target genes will provide opportunities for drug discovery and cancer prevention.
However, Houlston points out that it is more difficult to translate this knowledge into new therapies for cancer compared to IBD, because tumors are not static targets, but constantly evolve over time. “This is the challenge, whereas with something like Crohn’s disease and other intestinal diseases it doesn’t evolve,” he says.
 Getty Images
Getty ImagesLee is optimistic that Crick’s work in IBD will provide a template for how researchers can find new ways to understand the mechanisms involved in all kinds of autoimmune and inflammatory diseases. The institute’s scientists are now investigating other gene deserts that have been linked to conditions such as lupus, a disease in which the immune system damages the body’s tissues, leading to symptoms such as rash and fatigue.
Other research centers around the world, such as the University of Basel in Switzerland, are also investigating how single inherited mutations in gene deserts can lead to rare genetic diseases. Three years ago, Basel scientists discovers how one of these mutations could lead to babies being born with limb deformities due to its regulatory effects on a nearby gene.
Lee predicts that understanding the role of gene deserts will ultimately help improve the notoriously inefficient drug development process. “Creating new drugs for these diseases has been woefully unsuccessful,” he says. “Only about 10% of drugs that enter clinical trials are ever approved, so 90% of them fail because they don’t make people better. But if you know that your drug going into development actually targets a pathway supported by genetics, the chances of that drug actually being approved are at least somewhere between three- and five-fold greater.”